Facing down
dementia risk in Latinos
UC Davis is leading the largest study ever performed on cognitive impairment in Latinos, part of a larger research portfolio on diversity and disparities in Alzheimer’s and other dementias.
Latinos or Hispanics are the largest and fastest-growing ethnic group in California, and the fastest-growing minority in America’s aging population.They’re also half again more likely to suffer the brain-wasting effects of Alzheimer’s disease or other dementias as white people of similar age.
As such, Hispanic families are expected to bear a disproportionately large share of the nation’s substantial and ever-mounting burden of suffering due to Alzheimer’s and related dementias, which by 2050 could exceed 16 million Americans diagnosed with Alzheimer’s and $1 trillion in annual caregiving costs.
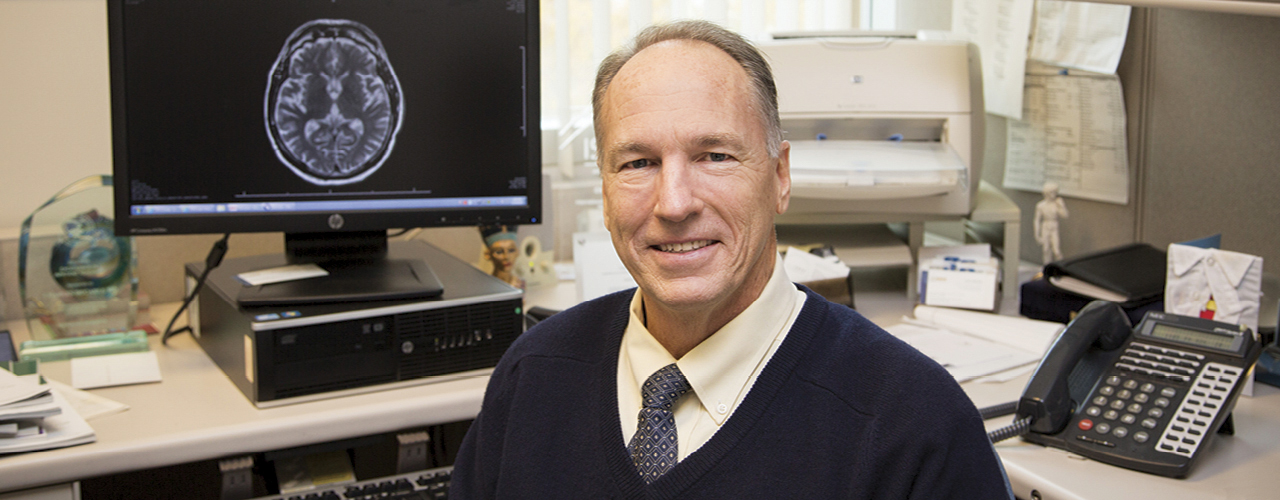
To help forestall this potential increase in dementia among Latinos, UC Davis Health recently added a new investigation of historic size and scope to its larger portfolio of current and past research on cognitive decline in ethnic populations. With support from a nearly $15 million National Institutes of Health grant, last fall the university launched a multicenter study that will represent the largest examination of Latinos with cognitive impairment ever performed, according to Charles DeCarli, M.D., co-principal investigator on the effort and director of the UC Davis Alzheimer’s Disease Center.
DeCarli and colleagues at the multidisciplinary Alzheimer’s center are now working with counterparts at nine institutions across the country to examine the biological underpinnings of stroke, mild cognitive impairment and dementia among Hispanics, and to pursue new therapeutic directions to reduce brain health disparities.
“Because Latinos are the fastest-growing minority population in our aging population, cognitive impairment in this group is really an important public health concern,” said DeCarli, a neurology professor and UC Davis Health’s Victor and Genevieve Orsi Endowed Chair in Alzheimer’s Research, who in 2010 earned the J. Allyn Taylor International Prize in Medicine honoring leading researchers in biology, medicine and imaging. “The new grant is a major effort that’s going to help us advance many interesting, critical lines of research in a very ethnically and genetically diverse population group.”
A uniquely diverse population
The UC Davis Alzheimer’s Disease Center is one of 27 nationwide designated by the NIH’s National Institute on Aging, and aims to translate research advances into improved diagnosis and treatment for patients — while focusing on the long-term goal of finding a way to prevent or cure the disease and other dementias. Its location in melting pot California (and additional state funding) allows researchers to study the effects of the disease on a uniquely diverse population, and over time the center has recruited its own diverse research cohort to help identify and clarify issues ripe for larger-scale exploration.
“Over the years, our center has moved in steps from a largely clinically-based program to one that’s also doing leading-edge, comprehensive assessments of community based studies to help understand aging and dementia risk factors in these diverse communities,” DeCarli said.
For the new $15 million effort, DeCarli and co-principal investigator Hector Gonzalez of UC San Diego will also draw on a cohort of more than 16,000 patients from the ongoing Hispanic Community Health Study/Study of Latinos (HCHS/SOL), a multicenter epidemiologic study primarily focused on cardiovascular and pulmonary diseases. An ancillary study, the Study of Latinos-Investigation of Neurocognitive Aging (SOL-INCA), is examining genetic and cardiovascular disease risk factors for neurocognitive deficits and will also provide important data for the research.
Variations in health, lifestyle and socioeconomic risk factors across racial groups likely account for most of the differences in risk of Alzheimer’s and other dementias by race, according to groups like the nonprofit Alzheimer’s Association. For one, health conditions such as cardiovascular disease, diabetes and obesity — all linked to increased dementia risk — are more prevalent in African-American and Hispanic people. Socioeconomic characteristics — such as greater exposure to early-life poverty, discrimination and other adversities — may increase risk in these communities as well.
Studying individuals from diverse backgrounds enables researchers at the UC Davis Alzheimer’s Disease Center to identify specific, possibly treatable risk factors to delay — and perhaps prevent — late-life dementia. Differences in ancestry may also be linked to differences in biological processes causing dementia, thereby leading to new discoveries about how to identify and possibly treat individuals at increased risk.
Cardiovascular risk, genetics and advanced imaging
The new UC Davis study entitled SOL-INCA-MRI will make use of leading-edge magnetic resonance imaging (MRI) techniques, which can help assess vascular brain injury and patterns of atrophy seen in various causes of dementia such as Alzheimer’s and vascular disease.
MRIs will be acquired at the partnering institutions and evaluated at UC Davis, where DeCarli also directs the UC Davis Imaging of Dementia and Aging (IDeA) laboratory at the university’s Center for Neuroscience in Davis. The long-running facility investigates the biological basis of neurodegenerative diseases and aging-related cognitive changes using techniques such as positron emission tomography (PET), MRI and functional MRI.
“Advanced neuroimaging techniques can help us to improve our understanding of the relationship between brain structure and function with aging and disease,” DeCarli said. “The information that we glean from imaging is going to help us better design and monitor new therapies.”
Another path of inquiry in the study explores the role of genetics in dementia among Latinos, a large group that’s marked by widespread intrapopulation ethnic and genetic diversity, as well as some mysterious contradictions that provoke further study. For example, the E4 variant of the APOE gene — already known to increase risk of late-onset Alzheimer’s disease — has been strongly implicated in increasing the risk of early-onset Alzheimer’s disease in non-Hispanic Caucasians. Paradoxically, some Hispanic ethnic groups have a very low frequency of the allele despite high rates of dementia, suggesting other mechanisms of disease. Identifying these other mechanisms may lead to new treatments.
Looking at early life experiences
The new study is one of several past and present efforts at UC Davis to zero in on causes and cures for Latinos and other ethnic groups that face higher prevalence of Alzheimer’s and related dementias. The Alzheimer’s Disease Center is currently partnering with the Kaiser Permanente Northern California Division of Research on other large, federally funded efforts as well, such as a long-term study of ethnic disparities in brain health and dementia funded with a five-year, $13 million NIA grant.
This study, named KHANDLE (Kaiser Healthy Aging and Diverse Life Experience), revisits physical exams conducted by Kaiser providers from the 1960s through the 1980s. Researchers will evaluate how risks and protective factors earlier in life — such as midlife vascular health, psychosocial conditions and early-life growth indicators — have influenced brain health and dementia risk among a large, ethnically diverse group of seniors. In particular, investigators are exploring how conditions earlier in life may play roles in racial and ethnic differences in dementia rates and risk factors for cognitive decline — an area that has not been well studied.
Kaiser researchers will conduct medical and cognitive evaluations and UC Davis researchers will provide MRI and PET scans for 1,800 white, black, Asian and Latino Kaiser members who previously participated in multiphasic exams, which use a variety of diagnostic procedures in the same screening program.
Variety of other efforts
KHANDLE is only one part of three diversity grants being performed in collaboration with the Kaiser Research Foundation, as well as ongoing research at the UC Davis Alzheimer’s Disease Center based on the center’s longitudinal cohort. Including SOL-INCA-MRI, the UC Davis center supports studies on cognitive aging and dementia risk among one of the largest and most diverse populations in the country.
Research from the UC Davis center’s diversity cohort has already led to new discoveries of dementia risk. A study led by Joshua Miller, Ph.D., discovered that more than 50 percent of individuals in the cohort were vitamin D insufficient, and that insufficiency was associated with decline in cognitive ability over time. Vitamin D levels were also significantly lower in Latinos and blacks than whites.
The research led to the successful award of a NIH clinical trial grant to test the efficacy of high-dose versus standard-dose vitamin D replacement on cognitive performance over time. The study, entitled “Phase II Randomized Clinical Trial of High-Dose Vitamin D Supplements in Older Adults,” involves 180 subjects and will last three years.
“The bulk of what is known about early-life risk factors for dementia and brain pathology is from studies of highly educated whites,” said Dan Mungas, Ph.D., the UC Davis Alzheimer’s Disease Center’s associate director. The neurology professor and longtime center researcher helped to introduce leading-edge neuropsychological testing methods that use statistical adjustments to account for cultural and linguistic differences — improving accuracy, and helping to reduce potential over-or under-diagnosis of dementias in non-white ethnic groups.
“Studies like our diversity cohort, the SOL-INCA-MRI, KHANDLE and our other Kaiser-associated research fill a much-needed gap in understanding dementia and brain aging in a group that is representative of the aging U.S. population,” he said.
Alzheimer’s dementia

age 65 and older has Alzheimer’s dementia

projected in number of Californians 65 or older with Alzheimer’s dementia within next decade
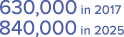
(about today’s population of San Francisco)

estimated number of Americans living with Alzheimer’s dementia in 2017

projected in 2050

estimated cost in 2017 of caring for those with Alzheimer’s and other dementias

by 2050 (in today’s dollars)