March 2020 - Presented by Dr. Anupam Mitra (Mentored by Dr. John Paul Graff)
A middle-aged patient with a history of HIV and poor adherence to antiretroviral therapy (HAART) presented to an outside institution with 1-week history of abdominal pain, nausea, and constipation.
CT scan of the abdomen revealed a large upper abdominal mass (20.1 x 12.4 x 9.5 cm) with small lucent areas, which were worrisome for a neoplastic process with focal areas of necrosis. Core biopsy was obtained, and initial pathology was interpreted as a CD10 positive high-grade B-cell lymphoma with very high Ki-67 approaching 100%. Patients was subsequently transferred to UC Davis Medical Center for higher level of care.
On admission, the patient continued to complain of abdominal discomfort and constipation. He denied B symptoms (fever, night sweats etc.). Patient was febrile, but alert and oriented. He appeared to be cachectic, irritable and was not in acute distress. His cardio-pulmonary examination was normal. Abdomen was firm and tender with bowel sounds present. There was no palpable lymphadenopathy or hepatosplenomegaly. His extremities were well perfused with no edema and no other significant physical findings.
His laboratory findings were notable for normocytic anemia (Hb: 10.6g/dl) and hypocalcemia (Ca: 7.8 mg/dl). A PET/CT was obtained which showed a large mesenteric abdominal mass (19.8 x 8.9 x 13.6 cm) with intense FDG avidity (Figure 1, mass designated by a red rectangle). Peripheral blood smear showed atypical lymphocytes (Figure 2). His initial abdominal mass biopsy was reviewed at UC Davis, which showed a highly pleomorphic population of large atypical cells with blast-like nuclear features including open immature chromatin and prominent nucleoli (Figure 3A). Tingible body macrophages were noted along with areas of increased apoptosis (Figure 3A, yellow arrows), and increased proliferation index as noted by Ki-67 stain (Figure 3B). A bone marrow biopsy was subsequently performed. The aspirate showed sheets of monotonous atypical appearing lymphocytes comprising approximately 40% of the marrow cellularity. The cells were highly pleomorphic with high N/C ratio, irregular nuclear contour, immature chromatin and prominent nucleoli. Prominent cytoplasmic vacuoles were seen (Figure 4). The core biopsy showed (Figure 5A) the same atypical lymphoid infiltrates, which by IHC staining were positive for CD20 (Figure 5B), PAX-5 (Figure 5C), BCL-6 (Figure 6A), CD10 (Figure 6B) and CMYC (Figure 6C). The cells were negative for TDT (Figure 7A), BCL-2 (Figure 7B) and BCL-1 (Figure 7C). However, the concurrent bone marrow flow cytometry showed no evidence of a monotypic B-cell population.
Figure 1
Figure 2
Figure 3
Figure 4
Figure 5
Figure 6
Figure 7








 Meet our Residency Program Director
Meet our Residency Program Director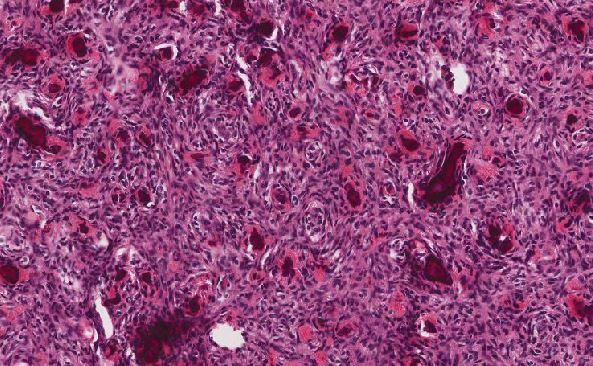
 LeShelle May
LeShelle May Chancellor Gary May
Chancellor Gary May