For many women who have undergone mastectomies, recreating a sense of normalcy and wholeness is an important part of their cancer journey.
Plastic surgery plays a key role as women get back to life after cancer treatment, and UC Davis Comprehensive Cancer Center has an exciting new option for patients.
The profunda artery perforator (PAP) flap technique for breast reconstruction is now available at UC Davis. The “PAP” is a blood vessel that runs through the thigh, and the “flap” is tissue taken from the inside of the upper thigh. The PAP flap gives women another option for natural reconstruction of the breast.
For many years, similar “all-natural” reconstruction methods such as the DIEP flap have been used to take tissue from the tummy to shape into a reconstructed breast. However, some women don’t have enough abdominal tissue to make a natural breast or have had certain prior abdominal surgeries that prevent the use of this tissue.
First patient
In 2023, breast cancer survivor Leslie Peek was the first patient at UC Davis Health to undergo the PAP flap procedure. At 43, the athletic mother of two was diagnosed with breast cancer during a routine mammogram.
Peek, who manages a career counseling team supporting pre-med students at UC Davis, knew it was important to research her medical options and gather as much information as possible. She decided a bilateral mastectomy (removing both breasts) would bring her the best peace of mind. The next choice involved exploring options for breast reconstruction.
“I knew my body would expand and contract as I enjoyed the rest of my life, so a natural reconstruction was appealing to me rather than breast implants,” Peek said. “However, there was not enough tissue in my abdomen for the traditional type of natural reconstruction.”
As a former triathlete and current strength-training coach, Peek doesn’t have a lot of extra fat and tissue to spare.
“However, my thighs turned out to be a rich source of tissue,” Peek said with a laugh.
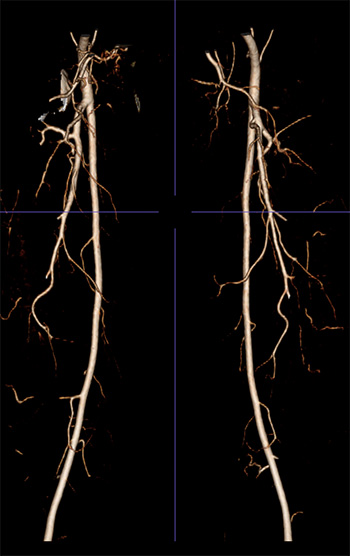
in the thigh used for planning PAP
flap surgery for breast reconstruction.
How it works
Small blood vessels that feed the thigh tissue are sewn to vessels in the chest to allow the tissue to survive in its new location. This involves connecting the small vessels (2 millimeters in diameter) under a microscope in what is called “microsurgery.” The PAP flap consists of skin and fat that is removed from the thigh and then molded into a breast shape.
Ara Salibian, a plastic surgeon and assistant professor in the UC Davis Department of Surgery, and his fellow plastic surgeon Michelle Zaldana-Flynn performed the PAP flap procedure on Peek.
Salibian is the new director of breast microsurgery at UC Davis. He recently joined UC Davis after completing a microsurgery fellowship at the Keck School of Medicine of USC. Salibian specializes in reconstructive microsurgery of the breast and lower extremities as well as lymphatic surgery, or microvascular surgery for the treatment of lymphedema.
“Many women do not want artificial breast implants that contain silicone or saline,” Salibian said. “The ability to offer this surgery has allowed us to expand the options for patients to have a natural breast reconstruction after a mastectomy who otherwise would not have been candidates for this type of procedure.”
Back to a busy life
Peek said she was up and walking around within a couple days of the PAP flap procedure and returned to caring for her kids at home and her career on campus within a few weeks.

daughter Genevieve and son Connor.
“The symmetry of my breasts is great and I feel like myself,” Peek said. “After the procedure, I felt hope for the first time — like I was going to be okay. For me this was the right choice.”
Peek is back doing what she enjoys, including playing softball and running. She’s even planning to enter the annual Davis Turkey Trot this year with her family — a Thanksgiving tradition she wasn’t able to take part in last year.
Leslie had an incredible attitude throughout her entire breast cancer treatment and breast reconstruction journey. It was an absolute pleasure to be a part of her treatment team and we are thrilled she can now get back to normal life,” said Salibian.
Peek said she credits Salibian for being a champion for breast cancer survivors and said the supportive environment created by her medical team, including Candice Sauder who performed her bilateral mastectomy, was truly remarkable.
“Breast cancer is challenging no matter what stage, but Leslie’s was caught early which gave her the most options for treatment and reconstruction,” Sauder said. “She really thought about her options and made the right choice for her. This is our goal for all of our patients, and she has done amazingly well.”
“My experience throughout treatment and follow-up care has made me even more proud to work for UC Davis,” Peek said. “I’m grateful because I know some women have to wait a couple of years to receive this type of reconstruction or are forced to travel a long way to receive it — and, yet, we have access to this innovative technology right here.”





