February 2020 - Presented by Dr. Alexander Ladenheim (Mentored by Dr. Maija Kiuru)
Clinical History
This is a 69-year-old South Asian female who presented with a rash of one month’s duration, long-standing neuropathy in a stocking glove distribution, polyarthritis, and fever. The cutaneous eruption consisted of violaceous to erythematous patches and plaques with associated edema, starting on the bilateral hands and feet and gradually spreading to the proximal limbs and trunk.
After admission, an extensive rheumatology workup was performed remarkable for a positive ANA, elevated CRP (60 mg/L) and ESR (35 mm/hr), negative lupus panel save for a slightly decreased C3 (80 mg/dL), negative rheumatoid arthritis workup, and negative ANCA screen. The rash and edema were initially thought to be drug-related, with the differential including connective tissue disease and infectious etiologies. The suspected offending medications were discontinued, and she received steroids and diphenhydramine with initial improvement in her erythema and edema.
One month later, the patient returned with similar symptoms. Punch biopsies of the rash were taken.
Microscopic Findings
Microscopically, there was a superficial and deep perivascular, prominent perineural and interstitial infiltrate of lymphocytes, plasma cells, and foamy histiocytes (Figures 1,2). Evidence of small vessel vasculitis was seen with leukocytoclasis and extravasation of erythrocytes (Figure 3).
Figure 1 Low power. A dermal perivascular, periadnexal, and perineural inflammatory infiltrate is seen
Figure 2 High power. Perineural inflammation.
Figure 3 Medium power. Leukocytoclastic vasculitis.

 Meet our Residency Program Director
Meet our Residency Program Director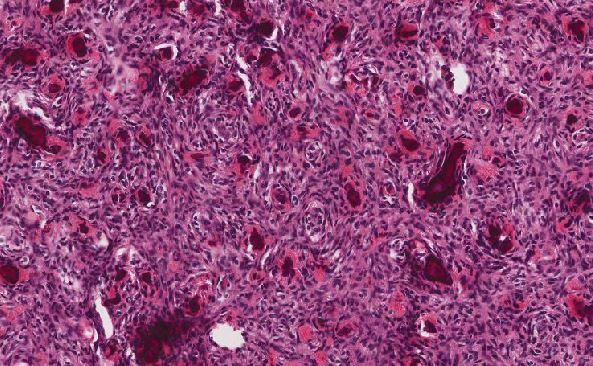
 LeShelle May
LeShelle May Chancellor Gary May
Chancellor Gary May